How to Ensure Your Progress Notes Meet Medical Necessity Standards
When it comes to psychotherapy progress notes, one important question is: Will my documentation hold up if an insurance company reviews it?
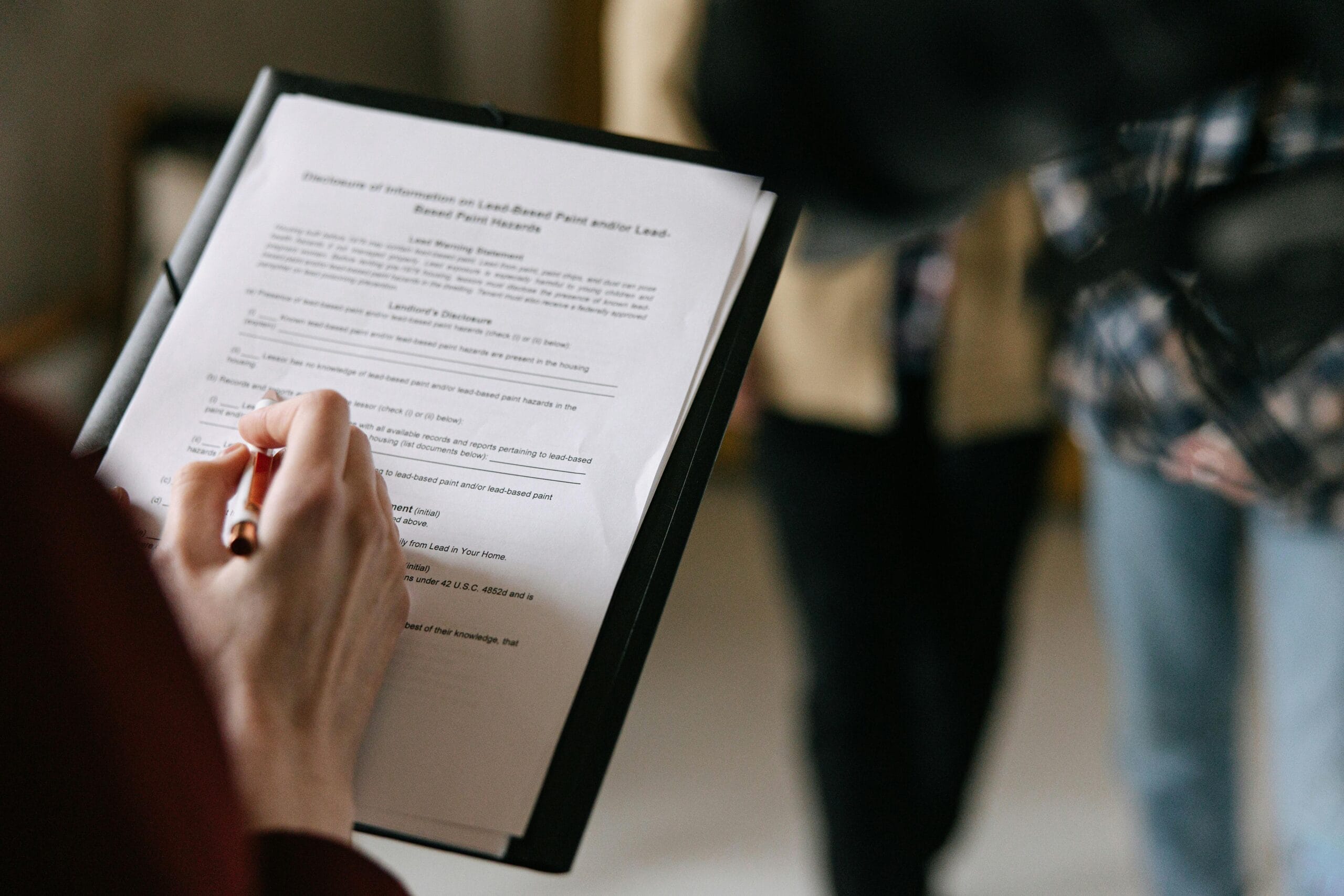
Payers — whether Medicare, Medicaid, or commercial insurers like UnitedHealthcare, Cigna, Aetna, or Blue Cross — require that notes demonstrate medical necessity. This isn’t just bureaucratic language. It’s about showing that the services you provide are directly tied to a patient’s diagnosis, symptoms, and functional improvement.
If documentation is incomplete, vague, or disconnected from the treatment plan, clinicians may face denials, delays, or requests for additional information. That’s why having a clear checklist is essential.
Below is a practical guide you can use to ensure your notes meet the standards for medical necessity.
📋 Medical Necessity Documentation Checklist
1. Basic Session Details
- Date of service (DOS)
- Start and stop times (required for time-based CPT codes)
- Service type (individual, family, group, telehealth, etc.)
- CPT code and place of service (e.g., POS 02/10 for telehealth)
- Attendees (for family or group sessions)
2. Diagnosis & Target Problems
- Active DSM-5/ICD-10 diagnosis
- Symptoms addressed during today’s session
- How those symptoms impair functioning (work, school, daily life, relationships)
3. Patient Status & Risk
- Brief mental status exam update
- Risk assessment (suicidality, self-harm, homicidality, safety plan if needed)
- Patient’s ability and readiness to participate in treatment
4. Link to Treatment Plan
- Goals and objectives worked on in today’s session
- Progress toward those goals (improved, unchanged, or regressed, with examples)
5. Interventions & Response
- Specific therapeutic techniques used (e.g., CBT cognitive restructuring, EMDR resourcing, supportive therapy)
- Patient’s response to the interventions (insights, behaviors, level of engagement)
6. Medical Necessity Statement
- A one-to-two sentence explanation connecting:
- The patient’s symptoms/impairments
- The clinician’s chosen interventions
- The expected improvement in functioning
Example:
“Today’s psychotherapy session was medically necessary to address persistent anxiety interfering with occupational performance. Exposure-based CBT was used to reduce avoidance behaviors and support the patient’s return to baseline work functioning.”
7. Plan / Next Steps
- Next session focus and frequency
- Homework or practice assignments
- Referrals or coordination with other providers
- Notes about discharge planning if appropriate
8. Telehealth (if applicable)
- Patient location
- Provider location
- Modality (audio-video, or audio-only if allowed)
- Patient’s consent to telehealth
9. Compliance Footer
- Clinician’s signature and credentials
- Date and time finalized
Why This Matters
Insurance reviewers are looking for more than a record of time spent. They want to see that:
- The service addressed an active diagnosis and functional impairment.
- Interventions were purposeful and clinically appropriate.
- The patient is making progress, or the clinician has a clear rationale for continued treatment.
When these elements are in place, your notes not only protect you from denials and audits, but also reflect high-quality, ethical care.
How Note Designer Helps
At Note Designer, we’ve built these requirements right into our progress note templates. Clinicians are guided to document start and stop times, link each note to treatment goals, and generate a concise medical necessity statement. The clinician can also easily customize their notes to more specifically comply with the particular insurance provider they are using.
Documentation should be clinically meaningful first, and insurance-compliant second — and with the right structure, you can achieve both.
For more reflections about Medical Necessity in psychotherapy practice, here is the link to my other post about this https://notedesigner.com/why-medical-necessity-matters-in-therapy-documentation/

Patricia C. Baldwin, Ph.D
Clinical Psychologist
President
Note Designer Inc.